Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting women of reproductive age. It is characterized by irregular menstrual cycles, excessive androgen levels, and polycystic ovaries. The exact cause of PCOS is not fully understood, but it is believed to involve a combination of genetic, environmental, and lifestyle factors, including insulin resistance and obesity.
Causes of PCOS
- Genetic Factors: PCOS tends to run in families, suggesting a genetic component.
- Insulin Resistance: Many women with PCOS have insulin resistance, leading to higher insulin levels, which can increase androgen production and exacerbate symptoms.
- Obesity: While not all women with PCOS are obese, obesity can worsen insulin resistance and symptoms.
Factors Worsening Symptoms
- Obesity: Increases insulin resistance and androgen levels, exacerbating symptoms like hirsutism and menstrual irregularities.
- Poor Diet and Sedentary Lifestyle: Can contribute to weight gain and insulin resistance.
Factors Improving Symptoms
- Weight Loss: Even modest weight loss can improve symptoms by reducing insulin resistance and restoring ovulation.
Healthy Diet and Regular - Exercise: Help manage weight and improve insulin sensitivity.
- Medications: Various medications can help manage symptoms and improve fertility.

PCOS and Fertility Challenges
PCOS is a leading cause of infertility due to irregular ovulation or anovulation (lack of ovulation). The hormonal imbalances in PCOS, particularly elevated androgens and insulin resistance, disrupt the normal development and release of eggs from the ovaries. This makes it difficult for women with PCOS to conceive naturally.
Medications for PCOS
- Metformin: Originally used for type 2 diabetes, metformin improves insulin sensitivity, which can help lower insulin and androgen levels, regularize menstrual cycles, and potentially restore ovulation.
- Clomiphene Citrate: Used to induce ovulation in women who wish to become pregnant.
- Hormonal Contraceptives: Birth control pills help regulate menstrual cycles, reduce androgen levels, and manage symptoms like acne and hirsutism.
- Anti-Androgens: Medications like spironolactone can reduce excessive hair growth and acne by blocking androgen effects.
Overall, managing PCOS requires a comprehensive approach, including lifestyle changes and medication, tailored to the individual’s symptoms and reproductive goals.
Insulin resistance plays a significant role in the development and exacerbation of Polycystic Ovary Syndrome (PCOS) symptoms. Here’s how it contributes to the condition:
Contribution of Insulin Resistance to PCOS Symptoms
- Increased Androgen Production: Insulin resistance leads to higher levels of insulin in the bloodstream. Elevated insulin levels can stimulate the ovaries to produce more androgens (male hormones), such as testosterone. This increase in androgens can cause symptoms like hirsutism (excessive hair growth), acne, and irregular menstrual cycles.
- Interference with Follicular Development: High insulin levels can disrupt the normal development of ovarian follicles, the sacs where eggs develop. This disruption can prevent ovulation, leading to irregular or absent menstrual periods, a hallmark of PCOS.
- Weight Gain and Obesity: Insulin resistance is often associated with weight gain, which can further exacerbate PCOS symptoms. Excess body fat can lead to even higher insulin levels, creating a vicious cycle that worsens the condition.
- Metabolic Complications: Women with PCOS and insulin resistance are at a higher risk of developing metabolic issues such as glucose intolerance, type 2 diabetes, and cardiovascular diseases. These metabolic complications can further impact overall health and exacerbate PCOS symptoms.
In summary, insulin resistance is a key factor in the pathophysiology of PCOS, contributing to both the reproductive and metabolic symptoms of the disorder. Managing insulin resistance through lifestyle changes and medications can help alleviate these symptoms and improve overall health outcomes for women with PCOS.
In the context of Polycystic Ovary Syndrome (PCOS), elevated insulin and androgen levels are closely related to the levels of sex hormone-binding globulin (SHBG), a protein that plays a critical role in regulating the bioavailability of sex hormones.

Relationship Between Insulin, Androgens, and SHBG
- Insulin and SHBG: High insulin levels, common in insulin resistance, can suppress the production of SHBG in the liver. This reduction in SHBG leads to an increase in the amount of free androgens in the bloodstream because SHBG binds to sex hormones like testosterone, reducing their bioavailability. When SHBG levels are low, more free testosterone is available, exacerbating symptoms of hyperandrogenism such as hirsutism and acne.
- Androgens and SHBG: Elevated androgen levels, a hallmark of PCOS, also contribute to lower SHBG levels. The liver’s production of SHBG is inhibited by high levels of androgens, which further increases the amount of free testosterone in circulation.
- Vicious Cycle: The interplay between elevated insulin and androgen levels creates a vicious cycle. Insulin resistance leads to hyperinsulinemia, which reduces SHBG production, increasing free androgen levels. The elevated androgens can further suppress SHBG production, perpetuating the cycle and worsening PCOS symptoms.
Understanding this relationship is crucial for managing PCOS, as treatments that improve insulin sensitivity (such as metformin) can help increase SHBG levels, thereby reducing free androgen levels and alleviating symptoms associated with hyperandrogenism.
Women with Polycystic Ovary Syndrome (PCOS) often face challenges related to egg quality, which can impact fertility. The relationship between PCOS and poor egg quality is complex and influenced by the hormonal imbalances characteristic of the condition.
How PCOS Affects Egg Quality
- Hormonal Imbalances: PCOS is marked by elevated levels of androgens and insulin, which can disrupt the normal development and maturation of eggs in the ovaries. This hormonal environment can lead to eggs that are less mature or have genetic abnormalities, affecting their quality and the chances of successful fertilization.
- Irregular Ovulation: Women with PCOS often experience irregular or absent ovulation due to hormonal imbalances. This irregularity can prevent the timely release of mature eggs, which is crucial for fertilization and successful pregnancy.
- Insulin Resistance: Many women with PCOS have insulin resistance, which can further affect egg quality. Insulin resistance is associated with metabolic disturbances that can impair the environment in which eggs develop, potentially leading to poorer quality eggs.
- Inflammation: Chronic low-grade inflammation, common in PCOS, can also negatively impact egg quality by creating an unfavorable environment for egg development.
Controversy and Complexity
The extent to which PCOS affects egg quality is debated. Some studies suggest that PCOS does not inherently affect egg quality, while others report poorer egg quality in women with PCOS compared to those without the condition. This discrepancy may be due to the diverse phenotypes and presentations of PCOS, which can vary widely among individuals.

Improving Egg Quality
- Lifestyle Changes: Weight management, a balanced diet, and regular exercise can help regulate hormones and potentially improve egg quality.
- Medications: Ovulation-inducing medications like Clomid or Letrozole may be used to stimulate ovulation and improve egg quality.
- Supplements: Certain supplements, such as CoQ10 and Omega-3 fatty acids, have been suggested to enhance egg quality.
Overall, while PCOS can present challenges to egg quality, individualized treatment plans focusing on lifestyle modifications and medical interventions can help improve fertility outcomes for women with this condition.
Lifestyle changes can significantly improve egg quality in women with Polycystic Ovary Syndrome (PCOS) by addressing the underlying hormonal imbalances and metabolic issues associated with the condition. Here are some key lifestyle modifications that can enhance egg quality:
Diet and Nutrition
- Low Glycemic Index Diet: Consuming foods with a low glycemic index helps regulate insulin levels, which can reduce androgen production and improve hormonal balance. This includes eating more vegetables, fruits, lean meats, and high-fiber grains while avoiding refined carbohydrates and sugary foods.
- Nutrient-Rich Foods: A balanced diet rich in antioxidants, vitamins, and minerals supports overall reproductive health. Foods like broccoli (high in folate), salmon (rich in omega-3 fatty acids), and Brazil nuts (high in selenium) can promote a healthy environment for egg production.
Physical Activity
- Regular Exercise: Engaging in regular physical activity helps improve insulin sensitivity, reduce stress, and balance hormone levels, which are crucial for healthy follicle development and ovulation. Exercise can also help manage weight, which is often a concern in PCOS.
- Strength Training: Incorporating slow, weighted workouts can build muscle mass, further enhancing insulin sensitivity and potentially improving egg quality.
Stress Management
- Reducing Stress: Chronic stress can negatively impact hormone levels and egg quality. Practices like meditation, yoga, and deep breathing exercises can help manage stress and improve overall reproductive health.
Weight Management
- Achieving a Healthy Weight: Maintaining a healthy body weight can reduce inflammation and oxidative stress, which are detrimental to egg quality. Weight loss, even in modest amounts, can improve insulin sensitivity and hormonal balance.
Supplements
- Inositol: This supplement, part of the B vitamin family, has been found to improve insulin sensitivity and egg quality. It is often recommended for women with PCOS to enhance ovulation and fertility.
- CoQ10 and Omega-3 Fatty Acids: These supplements have shown promise in supporting egg health and improving fertility outcomes in women with PCOS.
Overall, these lifestyle changes can create a more favorable hormonal and metabolic environment, improving egg quality and enhancing fertility in women with PCOS. It is important for individuals to consult with healthcare professionals to tailor these strategies to their specific needs and circumstances.
Benefits of Reducing Sugar and Carbohydrates
- Improved Insulin Sensitivity: Women with PCOS often have insulin resistance, meaning their bodies require more insulin to manage blood sugar levels. High insulin levels can lead to increased androgen production, which negatively impacts egg development and quality. By reducing sugar and carbohydrate intake, insulin levels can be stabilized, improving insulin sensitivity and reducing androgen levels.
- Hormonal Balance: Lowering sugar and refined carbohydrate consumption helps reduce insulin spikes, which in turn can help balance reproductive hormones. This balance is crucial for the proper maturation of eggs and regular ovulation, both of which are essential for high-quality eggs.
- Reduced Inflammation: High sugar diets can contribute to systemic inflammation, which is detrimental to egg quality. By minimizing sugar intake, inflammation levels can decrease, creating a healthier environment for egg development.
- Weight Management: Many women with PCOS struggle with weight gain due to insulin resistance. Reducing sugar and carbohydrate intake can aid in weight loss, which is associated with improved fertility outcomes, including better egg quality and increased ovulation rates.
Enhanced Ovulatory - Function: Low-carbohydrate diets have been shown to improve ovulation function in women with PCOS, which is directly linked to better egg quality and increased chances of conception.
Overall, these dietary changes can help create a more favorable hormonal and metabolic environment, improving egg quality and enhancing fertility in women with PCOS. It is important for individuals to consult healthcare professionals or dietitians to tailor these dietary strategies to their specific needs.
Insulin resistance contributes to poor egg quality in women with Polycystic Ovary Syndrome (PCOS)
- Hormonal Imbalance: Insulin resistance leads to elevated insulin levels, which can stimulate the ovaries to produce more androgens, such as testosterone. This hormonal imbalance disrupts the normal development and maturation of eggs, resulting in poorer egg quality.
- Anovulation: Insulin resistance is associated with anovulation, where eggs do not mature properly or are not released from the ovaries. This lack of ovulation can lead to the accumulation of immature eggs, which are often of lower quality.
- Ovarian Environment: The excess insulin and androgens create an unfavorable environment within the ovaries, which can impair the development of healthy eggs. This can lead to eggs that are less mature or have genetic abnormalities, reducing their potential for successful fertilization and implantation.
- Inflammation and Oxidative Stress: Insulin resistance is often associated with increased inflammation and oxidative stress, both of which can negatively impact egg quality by damaging the cellular environment necessary for proper egg development.
Overall, managing insulin resistance through lifestyle changes and medications can help improve egg quality in women with PCOS by restoring hormonal balance and creating a healthier ovarian environment.

How Acupuncture, Low-Level Light Therapy, Customized Herbal Medicine, and Nutraceuticals Improve PCOS Parameters and Facilitate Conception
Polycystic Ovary Syndrome (PCOS) affects approximately 5-10% of women of reproductive age, making it one of the most common causes of anovulatory infertility. Characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology, PCOS also often coexists with metabolic disturbances such as insulin resistance, obesity, and dyslipidemia. Integrative approaches, including acupuncture, low-level light therapy, customized herbal medicine, and nutraceuticals, have demonstrated potential in improving PCOS-related parameters and supporting conception.
The Role of Acupuncture in PCOS Management
Acupuncture positively influences reproductive and metabolic markers in PCOS patients by modulating the hypothalamic-pituitary-ovarian (HPO) axis, enhancing blood flow, and reducing systemic inflammation. Specific benefits include:
- Regulation of Hormonal Imbalances: Acupuncture stimulates the release of β-endorphins, which regulate gonadotropin-releasing hormone (GnRH) secretion. This, in turn, helps normalize luteinizing hormone (LH) and follicle-stimulating hormone (FSH) ratios, critical for ovulation. Studies demonstrate improved menstrual regularity and ovulatory function with regular sessions. (Stener-Victorin et al., 2008)
- Improvement in Insulin Sensitivity: Research indicates that acupuncture can enhance insulin sensitivity by affecting glucose metabolism and improving lipid profiles. (Johansson et al., 2013)
- Reduction in Stress and Anxiety: PCOS is associated with increased psychological stress, which can exacerbate symptoms. Acupuncture’s calming effects lower cortisol levels, contributing to improved overall hormonal balance. (Liu et al., 2016)
Low-Level Light Therapy for PCOS
Low-level light therapy (LLLT) is a non-invasive modality that uses specific wavelengths of light to promote cellular function and reduce inflammation. For PCOS patients, LLLT offers the following benefits:
- Improved Cellular Energy Production: LLLT enhances mitochondrial activity, which can improve ovarian function and overall energy metabolism.
- Reduction in Inflammation: Chronic low-grade inflammation is a hallmark of PCOS. LLLT’s anti-inflammatory effects help reduce oxidative stress and inflammatory markers, improving metabolic and hormonal parameters. (Hamblin et al., 2017)
- Enhanced Blood Flow: By increasing local circulation, LLLT supports ovarian health and follicular development, facilitating ovulation.
Customized Herbal Medicine for PCOS
Traditional Chinese Medicine (TCM) views PCOS as a result of imbalances such as dampness, stagnation, and deficiency. Herbal medicine formulas are tailored to address these specific patterns and support reproductive and metabolic health. By focusing on the patient’s unique presentation, herbal medicine helps regulate menstrual cycles, balance hormones, and enhance ovulatory function. Customized formulas ensure optimal outcomes by targeting individual needs.
Nutraceuticals in PCOS Management
Nutraceuticals are dietary supplements with therapeutic effects that target the metabolic and hormonal dysregulation of PCOS. Evidence-based options include:
- Inositol: Myo-inositol and D-chiro-inositol improve insulin sensitivity, restore ovulation, and reduce hyperandrogenism. (Lagana et al., 2018)
- Omega-3 Fatty Acids: Omega-3 supplementation reduces inflammation, improves lipid profiles, and may enhance ovulatory function.
- Vitamin D: Vitamin D deficiency is prevalent in PCOS and linked to insulin resistance and anovulation. Supplementation helps improve these parameters. (Pal et al., 2018)
- N-acetylcysteine (NAC): NAC improves insulin resistance, reduces testosterone levels, and supports ovulation. (Thakker et al., 2015)
Integrative Approach to Conception
Combining acupuncture, low-level light therapy, customized herbal medicine, and nutraceuticals provides a synergistic approach to addressing the multifaceted nature of PCOS. This integrative method:
- Improves Ovulatory Cycles: Acupuncture and herbal medicine regulate the menstrual cycle, while inositol and NAC support ovulatory function.
- Reduces Androgen Excess: Herbal medicine and nutraceuticals like omega-3s lower androgen levels, improving fertility.
- Enhances Metabolic Health: Insulin sensitivity is improved through acupuncture, inositol, and tailored herbal formulas.
- Addresses Individual Needs: Customization ensures the treatment aligns with the patient’s unique pattern and presentation, maximizing efficacy.

Conclusion
PCOS-related infertility treatment requires a multidimensional approach for effective management. Acupuncture, low-level light therapy, customized herbal medicine, and nutraceuticals provide evidence-based interventions to improve hormonal, metabolic, and psychological parameters, ultimately enhancing fertility outcomes. By addressing the root causes and symptoms of PCOS, these therapies pave the way for successful conception and improved reproductive health.
References
- Johansson, J., et al. (2013). “Effect of acupuncture on insulin sensitivity and lipid metabolism in women with PCOS.” American Journal of Physiology-Endocrinology and Metabolism.
- Lagana, A. S., et al. (2018). “Myo-inositol in the treatment of polycystic ovary syndrome: a systematic review.” Obstetrics & Gynecology International.
- Liu, Z., et al. (2016). “The efficacy of acupuncture in managing anxiety in patients with PCOS: A randomized controlled trial.” Journal of Psychosomatic Obstetrics & Gynecology.
- Pal, L., et al. (2018). “Vitamin D supplementation and reproductive outcomes in PCOS: A meta-analysis.” Human Reproduction.
- Stener-Victorin, E., et al. (2008). “Acupuncture for the treatment of PCOS: A review of the literature.” Human Reproduction Update.
- Hamblin, M. R., et al. (2017). “Mechanisms and applications of low-level light therapy.” Lasers in Surgery and Medicine.
- Thakker, D., et al. (2015). “N-acetylcysteine in PCOS: A meta-analysis of randomized controlled trials.” Gynecological Endocrinology.
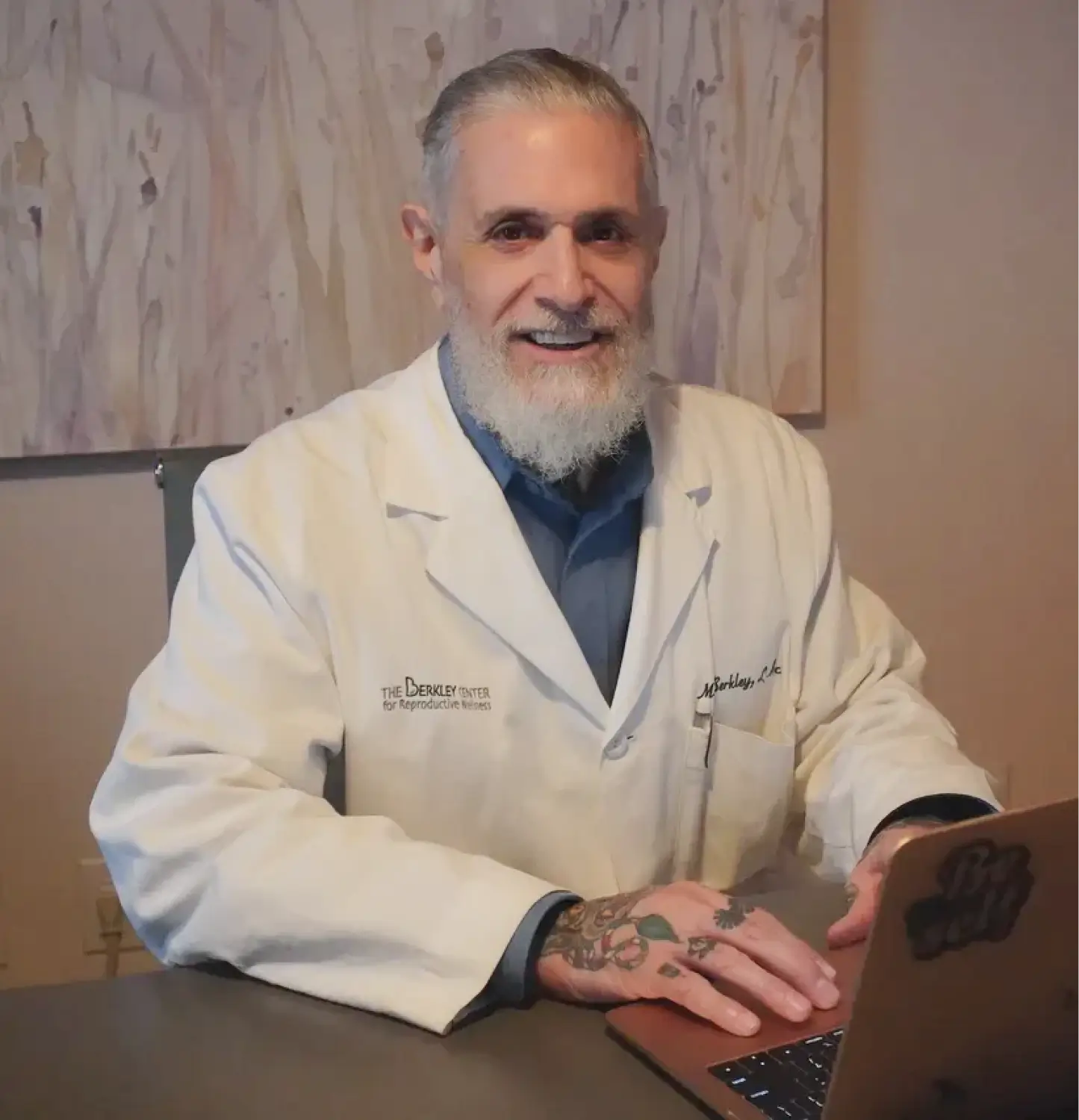
For more information or to schedule a consultation at The Berkley Center for Reproductive Wellness, please contact us at 212-685-0985 or visit our clinic at 16 East 40th Street, 4th floor, New York, NY 10016.
www.berkleycenter.com