Frequent urinary tract infections (UTIs) after intercourse, often called postcoital cystitis or “honeymoon cystitis,” are a common issue, particularly in women, due to anatomical, physiological, and behavioral factors. The primary cause is the introduction of bacteria into the urinary tract during sexual activity, compounded by individual predispositions. Let’s break down the mechanisms, contributing factors, and why this happens repeatedly.
Primary Cause: Bacterial Introduction
- Mechanism: Sexual intercourse can mechanically push bacteria from the vaginal, perineal, or anal areas into the urethra, the tube leading to the bladder.
- Key Culprit: Escherichia coli (E. coli), a common gut bacterium, accounts for 75-90% of UTIs. It thrives in the perineal region and can migrate during sex.
- Anatomy: Women are more prone because their urethra is short (~4 cm) compared to men (~20 cm), allowing bacteria a quicker path to the bladder.
Why Post-Intercourse Specifically?
- Urethral Trauma or Irritation:
Friction during sex can mildly irritate the urethral opening, making it easier for bacteria to adhere and invade the mucosal lining. Vigorous or prolonged activity may exacerbate this.
Movement during intercourse shifts bacteria from the anus or vagina toward the urethra. Partner’s skin or fluids can also introduce bacteria, though this is less common than self-contamination.
Pressure on the bladder during sex may prevent complete emptying, leaving residual urine—a breeding ground for bacteria. Delayed urination post-sex allows bacteria time to colonize before being flushed out.

Contributing Factors to Frequent UTIs
Beyond the act itself, several factors increase susceptibility or recurrence:
Anatomical Predisposition
- A shorter distance between the urethra and anus (common variation) facilitates bacterial migration.
- Urethral hypermobility or a low-lying bladder neck may heighten exposure during sex.
Hormonal Influence
- Low Estrogen: Postmenopausal women or those on certain contraceptives (e.g., low-dose pills) have thinner vaginal and urethral linings, reducing natural defenses (e.g., protective mucus).
- Estrogen supports lactobacilli, good bacteria that outcompete pathogens like E. coli.
Hydration and Voiding Habits:
- Infrequent urination or dehydration concentrates urine, reducing its antibacterial flush effect.
- Not urinating after sex lets bacteria linger in the bladder.
Immune or Microbial Balance:
- Weakened immunity (e.g., stress, illness) impairs the body’s ability to fight off invading bacteria.
- Vaginal dysbiosis (e.g., from antibiotics or spermicides) reduces protective flora, letting E. coli dominate.
Sexual Practices:
- Use of spermicides (e.g., diaphragms with spermicide) kills beneficial bacteria, increasing UTI risk.
- Anal-to-vaginal contact (intentional or accidental) directly transfers E. coli.
- Frequent intercourse amplifies exposure over time.
Underlying Conditions:
- Bladder Dysfunction: Incomplete emptying or reflux (vesicoureteral reflux) traps bacteria.
- Kidney Stones or Structural Issues: Rare, but can harbor bacteria, leading to recurrent infections.
- Diabetes: High urine glucose feeds bacterial growth.
Why Frequent or Recurrent?
- Biofilm Formation: E. coli can form protective layers in the bladder, resisting antibiotics and the immune system, leading to repeat infections.
- Genetic Susceptibility: Some individuals have more adhesive receptors (e.g., P-fimbriae binding sites) on urothelial cells, making E. coli stickier and harder to flush out.
- Cycle of Irritation: Each UTI inflames the bladder, potentially making it more vulnerable to the next infection if not fully healed.

Symptoms of Postcoital UTIs
- Burning during urination
- Frequent urge to pee with little output
- Cloudy or bloody urine
- Lower abdominal discomfort
- Onset typically within 24-48 hours post-intercourse
Prevention Strategies
To break the cycle:
- Urinate Before and After Sex: Flushes bacteria from the urethra.
- Hydrate Well: Dilutes urine and promotes frequent voiding.
- Wipe Front to Back: Prevents anal bacteria from reaching the urethra.
- Avoid Irritants: Skip spermicides, douches, or harsh soaps that disrupt vaginal flora.
- Consider Lubricants: Reduces urethral friction if dryness is an issue.
- Post-Sex Hygiene: Gentle cleaning (water, no harsh products) for both partners.
- Medical Options: Low-dose antibiotics (e.g., nitrofurantoin post-sex) or cranberry supplements (controversial but may help some) if recurrent.
When to Seek Help
UTIs persist despite prevention. Symptoms escalate (fever, back pain)—may indicate kidney involvement (pyelonephritis).
Recurrence suggests an underlying issue (e.g., anatomical anomaly, resistant bacteria), warranting a urologist visit or tests like a cystoscopy.
Conclusion
Frequent UTIs post-intercourse stem from bacteria (usually E. coli) being pushed into the urethra during sex, amplified by factors like anatomy, hormones, or habits. For some, it’s a one-off irritation; for others, it’s a recurring battle due to susceptibility or incomplete clearance. Simple steps like peeing after sex can help, but persistent cases need medical digging. Does this match your experience, or want to explore prevention in more depth?
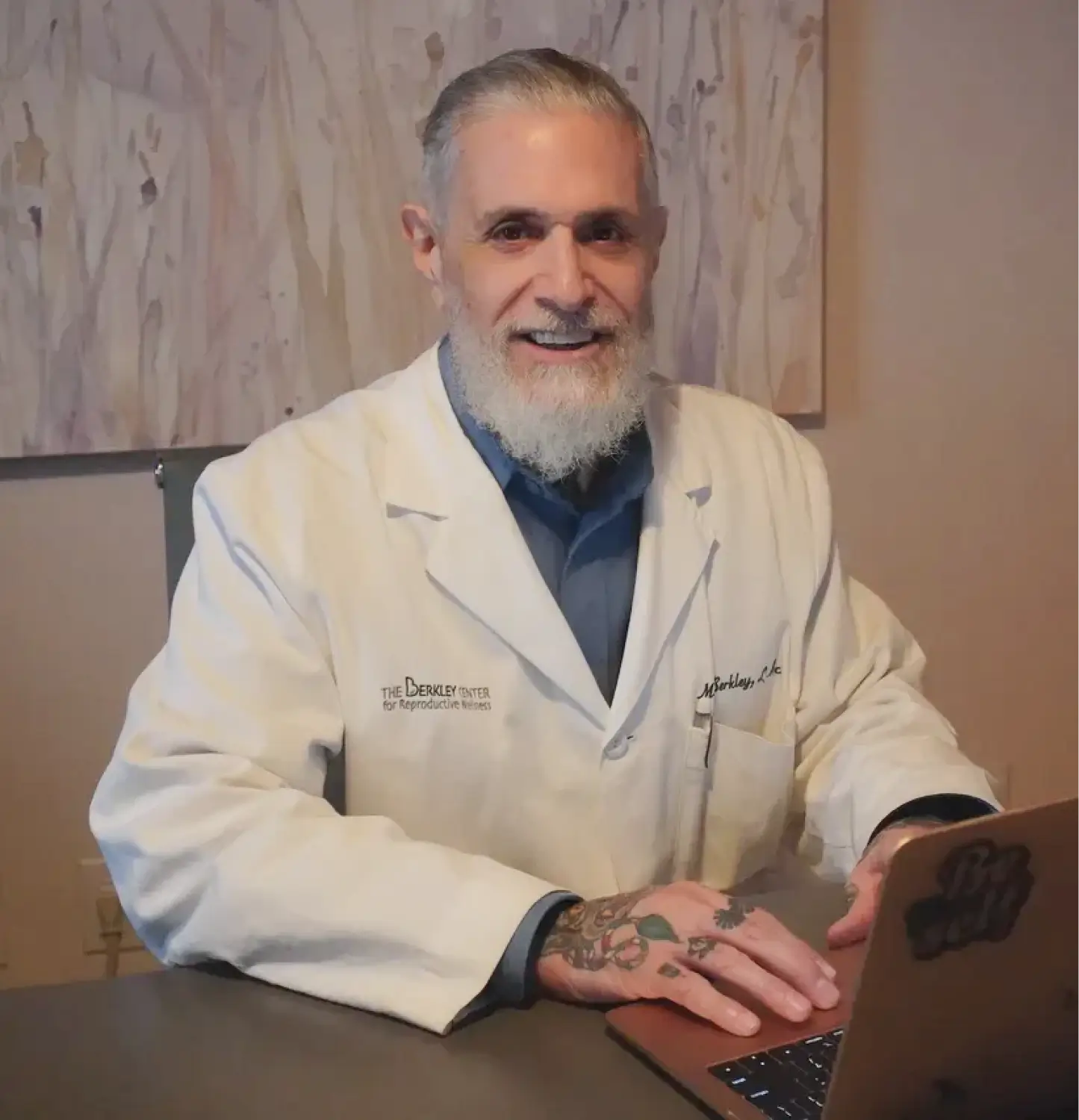
For more information or to schedule a consultation at The Berkley Center for Reproductive Wellness, please contact us at 212-685-0985 or visit our reproductive fertility center at 16 East 40th Street, 4th floor, New York, NY 10016.